Nephrology & Hypertension
Dr Daniel
Schwartz
Dr Schwartz is passionate about managing chronic kidney disease and supporting his patients to achieve the best clinical outcomes.

ClinIcAL Focus
Areas of clinical focus & experience
Chronic Kidney Disease
Dr Schwartz works with his patients to aggressively manage risk factors for progression of disease, with a focus on lifestyle modification & evidence-based pharmaceutical intervention.
Hypertension
As part of chronic kidney disease care, Dr Schwartz addresses difficult to control hypertension.
Cardio-Metabolic Optimization
Kidney disease is part of a spectrum of a cardio-metabolic disorder. Dr Schwartz addresses the entire spectrum of disease through direct management or appropriate referral.
Peritoneal Dialysis
As director of the Fraser Health home dialysis program, Dr Schwartz is a passionate supporter of independent dialysis.
Interventional Nephrology
Dr Schwartz performs procedures for patients within the kidney program.
Acute Nephrology Care
Dr Schwartz provides on-call nephrology services as part of the Fraser Health Kidney program.
New Patients
Consultations require a referral from your primary care provide or specialist
Virtual visit, or in person at #100-200 Keary Street, New Westminster, BC | Map
P (604) 516-7774
F (604) 516-7764
Kidney Care Centre
Requires a referral from Dr. Schwartz’s outpatient office
#217 – 610 Sixth St (Royal City Centre Mall), New Westminster, BC
(604) 549-6300
Hemodialysis
Royal Columbian Hemodialysis Dialysis Unit | Map
(604) 520-4582
Peritoneal Dialysis
Abbotsford Regional Hospital Peritoneal Dialysis Unit | Map
(604) 851-4769
Royal Columbian Peritoneal Dialysis Unit | Map
(604) 520-4503
Expertise
Dr Schwartz has a wide-range of professional interests & experience.
Dr Schwartz is a nephrologist and medical lead of the Fraser Health home dialysis program. He is also Clinical Assistant Professor of Medicine at the University of British Columbia. His clinical interests are focused on peritoneal dialysis, interventional nephrology and late stage chronic kidney disease (CKD) management.
He also has a keen interest in knowledge translation at the point of care and the intersection of information technology with clinical medicine. He is the creator of many online and mobile medical education offerings including QxMD, and works with great medical education partners such as Lyrn.
- Chronic Disease Management
- Medical Information Technology
- Procedural MEDICINE
- MEDICAL EDUCATION

Offering remote & virtual consultations to allow more convenient access to kidney care.
RECENT THOUGHTS
Reducing the Cost of Pharmaceutical Drugs in Canada
Access to CareReducing the Cost of Pharmaceuticals in Canada Canada is well-known for its universal healthcare system, which provides all citizens and permanent residents with access to medically necessary hospital and physician services without direct charges at the...
Tips for starting an SGLT2 inhibitor
SGLT2i inhibitors (eg empagliflozin, dapagliflozin, canagliflozin) have a phenomenal evidence base and have been shown to be beneficial in diabetes, heart disease (particularly heart failure) and kidney disease.
Achieving a good start is important.
10 Opportunities to increase access to physicians through IT efficiencies
In Canada we are facing unprecedented barriers in accessing physicians (both primary care & specialty care. Many barriers exist, but lack of time is a major one.
Huge opportunity to enhance & modify IT processes to give healthcare providers back time that can then be reinvested in patient care. HCP time is a zero-sum game.
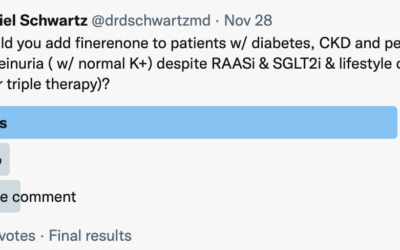
Should patients w/ diabetes, CKD and proteinuria despite RAASi & SGLT2i be considered for add-on therapy with finerenone (triple therapy)?
Would you add finerenone to patients with diabetes, CKD and persistent proteinuria despite RAASi & SGLT2i & lifestyle changes (ie offer triple therapy)?
Most impactful clinical trials: slowing progression of chronic kidney disease
This is a highly subjective list, but these trials have been included as they have had a meaningful impact on guidelines, patients and clinicians at a global scale.
7 ways the EMPA-KIDNEY trial will impact clinical care in CKD
EMPA-KIDNEY was a clinical trial testing whether taking a single pill of empagliflozin every day prevents worsening of kidney disease or deaths from heart disease in people who have chronic kidney disease (CKD). The trial was stopped early due to evidence of efficacy and was reported in November 2022 at the American Society of Nephrology ‘Kidney Week’ meeting and simultaneously published in the New England Journal of Medicine
Personalized decision support and the move from NNT to iNNT
The SPRINT trial made waves in the field of hypertension, showing evidence for reduced hard clinical endpoints (a combined outcome of myocardial infarction, acute coronary syndrome not resulting in myocardial infarction, stroke, acute decompensated heart failure, or death from cardiovascular causes) in those patients with a BP target of 120 mm Hg systolic.
Will SPRINT Change Our Systolic BP Target in Hypertensive Patients from 140 to 120 mm Hg?
At last week’s Medicine rounds at the Royal Columbia Hospital, I presented the results from the recently published SPRINT trial. In short, my thoughts are that…
Preventative Foot Care Project May Reduce Amputations, Hospitalization and Length of Stay in ESRD
At the 2015 BC Kidney Days, Dr. Shaoyee Yao and Sarah Lacroix present the preliminary results from a quality improvement project designed to reduce preventable complications from lower extremity wounds in patients on dialysis.